Understanding the Role of a Thoracic Specialist
The field of medicine encompasses a myriad of specialties, each contributing uniquely to patient care. Among these, the thoracic specialist plays a pivotal role in diagnosing and treating conditions that affect the organs within the thorax, primarily focusing on the lungs and heart. This article delves into the intricate details of the thoracic specialty, examining the qualifications, procedures, and the impact these specialists have on enhancing patient outcomes.
What is a Thoracic Specialist?
A thoracic specialist, also known as a thoracic surgeon or pulmonologist, is a physician who has undergone extensive education and training to provide expert care for patients with thoracic diseases. They are often involved in the surgical treatment of thoracic conditions, while some may specialize in non-surgical management, such as respiratory conditions. Their expertise typically covers a range of areas, including:
- Lung Cancer Treatment
- Esophageal Disorders
- Minimally Invasive Surgical Techniques
- Pleural Diseases
- Congenital Disorders of the Chest
Training and Qualifications
Becoming a thoracic specialist requires a significant commitment to education and specialized training. The pathway generally includes:
- Undergraduate Education: This typically involves completing a bachelor's degree with a focus on science-related courses.
- Medical School: Aspiring thoracic specialists must then attend a medical school, earning a Doctor of Medicine (MD) or Doctor of Osteopathic Medicine (DO) degree.
- Residency Training: After medical school, graduates complete a general surgery residency, which lasts about five years.
- Fellowship Training: Following residency, physicians undergo further training in thoracic surgery or pulmonary medicine through a fellowship program that can last an additional 1-3 years.
- Board Certification: Finally, they must pass rigorous examinations to become board-certified in thoracic surgery or pulmonary medicine.
Common Conditions Treated by a Thoracic Specialist
A thoracic specialist manages a variety of conditions impacting the thoracic region. Some common conditions include:
- Lung Cancer: They conduct diagnostic tests, create treatment plans, and perform surgery when necessary.
- Chronic Obstructive Pulmonary Disease (COPD): They manage symptoms through medications, therapies, and, in some cases, surgical interventions.
- Esophageal Cancer: They may perform surgeries such as esophagectomy to treat this often aggressive cancer.
- Trauma to the Chest: They are equipped to handle severe injuries that may require immediate surgical intervention.
- Infectious Diseases: This includes conditions like pneumonia or lung abscesses that may require complex treatment strategies.
Diagnostic Procedures Performed by a Thoracic Specialist
Diagnosing thoracic conditions often involves an array of advanced procedures. Some of the most commonly used diagnostic techniques include:
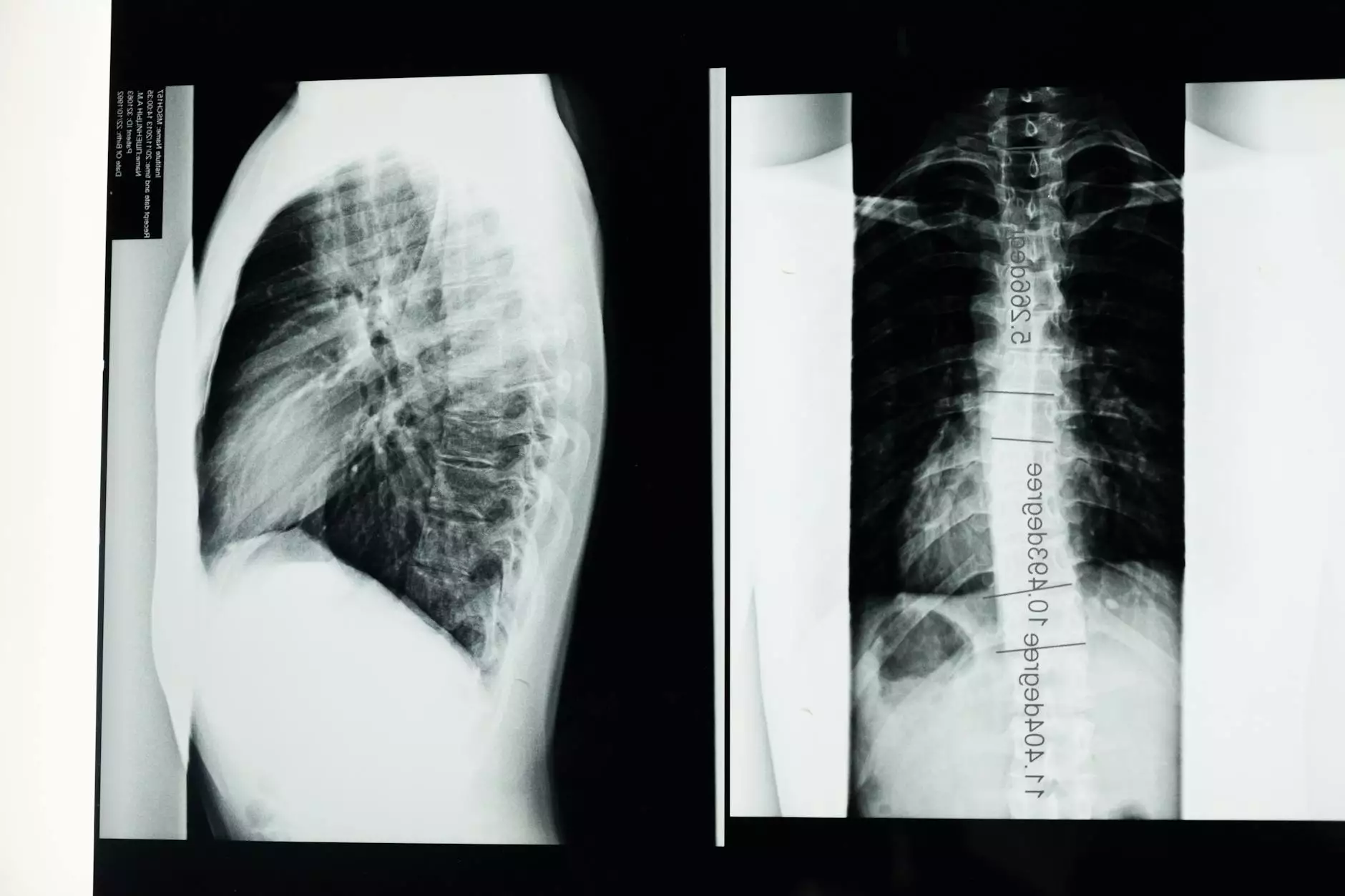
- Chest X-Rays: A fundamental imaging technique to identify any abnormalities in the lungs and surrounding structures.
- CT Scans: Provides detailed images of the chest, helping in the diagnosis of complex conditions such as tumors.
- Bronchoscopy: A procedure that allows the thoracic specialist to view the airways and collect tissue samples for biopsy.
- Thoracentesis: A minimally invasive procedure to remove excess fluid from the pleural space for analysis.
- Pulmonary Function Tests: These tests measure lung capacity and efficiency to diagnose conditions like asthma or COPD.
Surgical Interventions by Thoracic Specialists
One of the critical roles of a thoracic specialist is to perform surgeries that are essential for treating various thoracic conditions. Some of the most common surgical procedures include:
- Lobectomy: Surgical removal of a lobe of the lung, commonly performed for lung cancer.
- Video-Assisted Thoracoscopic Surgery (VATS): A minimally invasive surgery allowing the specialist to perform operations through small incisions, leading to quicker recovery.
- Esophagectomy: Removal of part or all of the esophagus, usually due to cancer.
- Pneumonectomy: Removal of an entire lung, often considered in severe cases of lung disease.
- Chest Wall Reconstruction: Repairing the chest wall after trauma or surgery.
The Importance of Multidisciplinary Teams
A thoracic specialist often works as part of a multidimensional healthcare team. Collaboration between various specialists ensures comprehensive care for patients. This team may include:
- Medical Oncologists: Specialists in cancer treatment who assess and provide therapies for the cancer patient.
- Radiologists: Experts who interpret imaging studies and guide treatment planning.
- Respiratory Therapists: Professionals who assist with respiratory care and rehabilitation.
- Nurses: Vital team members who provide bedside care and support to patients pre and post-procedure.
- Nutritionists: Specialists who offer dietary advice, critical for recovery and overall health.
Patient Experiences and Outcomes
Patients who consult a thoracic specialist often go through a life-changing experience. The journey from diagnosis to treatment involves emotional, physical, and financial aspects. Understanding the expected outcomes based on current medical advancements provides hope and clarity for patients and their families. Some positive patient outcomes associated with the care of a thoracic specialist include:
- Improved Survival Rates: Timely interventions by thoracic specialists significantly increase the chances of survival, particularly in cancer cases.
- Enhanced Quality of Life: Effective treatment strategies lead to better management of symptoms and improved functional status.
- Personalized Care Plans: Thoracic specialists create individualized treatment plans tailored to each patient's specific needs.
The Future of Thoracic Medicine
As medical technology advances, the future for thoracic specialists looks promising. Innovations such as robotic-assisted surgeries, advancements in minimally invasive techniques, and improved imaging modalities are on the rise. Research is continuously evolving, leading to:
- Targeted Therapies: These focus on specific characteristics of cancer cells, improving treatment efficacy.
- Telemedicine: Enhancing accessibility for patients needing guidance from thoracic specialists from the comfort of their homes.
- Emerging Technologies: Use of artificial intelligence for predictive analytics in patient care, improving diagnostics and treatment plans.
Conclusion: The Vital Role of Thoracic Specialists
In conclusion, a thoracic specialist is crucial in diagnosing, treating, and managing conditions of the thorax. Their rigorous training, coupled with their passion for patient care, positions them as essential members in the healthcare ecosystem. By staying abreast of technological advancements and continuously improving treatment paradigms, thoracic specialists contribute significantly to improving patient outcomes. Individuals facing challenges related to thoracic health should seek the expertise of these specialists to ensure they receive the best possible care and support on their journey to recovery.
Contacting a Thoracic Specialist
If you or a loved one is experiencing symptoms related to the thorax, don’t hesitate to consult with a thoracic specialist. At Neumark Surgery, our team of dedicated specialists is ready to assist with cutting-edge treatment options tailored to your unique health needs. Learn more about the specialized care we provide by visiting neumarksurgery.com.